

Click here
to view this message in a web browser
 |
||
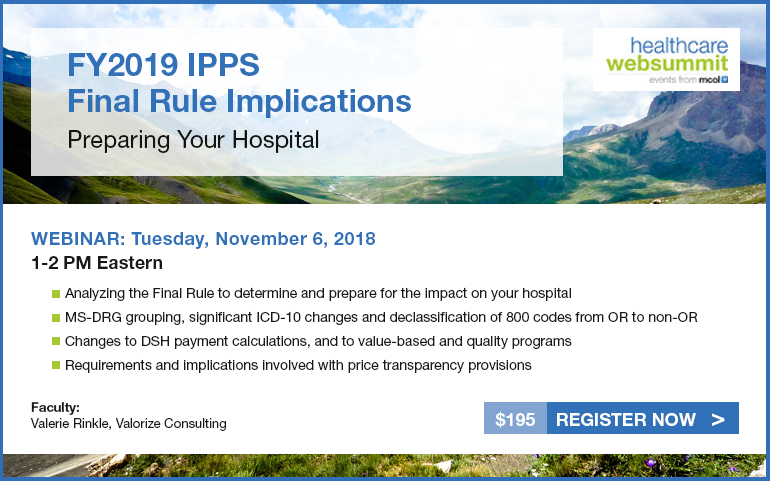
| FY2019 IPPS Final Rule Implications: Preparing Your Hospital | ||
|
The IPPS Fiscal Year 2019
Final Rule addresses price transparency requirements with numerous
implications for hospitals going forward, as well as changes impacting
value-based and quality programs, DSH calculations, new adjustment
factors for hospital-acquired conditions and hospital readmission
reduction program, MS-DRG grouping and significant ICD-10 modifications,
reductions of reporting measures, payment rate update factors and much
more. CMS pays acute care hospitals for inpatient stays under the IPPS. Under this payment system, CMS sets base payment rates prospectively for inpatient stays based on the patient’s diagnosis and severity of illness. Subject to certain adjustments, a hospital receives a single payment for the case based on Medicare Severity Diagnosis-Related Groups (MS-DRGs) – which are assigned at discharge. This session addresses how to evaluate the impact of the fiscal year 2019 Inpatient PPS Final rule on your hospital, with respect to coding, payment calculations, reporting measures, legislative and regulatory issues and the longer range implications of price transparency. Please join us on Tuesday November 6, 2018, at 1 PM Eastern as Valerie Rinkle presents detailed discussion and analysis of provisions and implications of the FY2019 IPPS Final Rule. Click here for detailed information and to register or call 209.577.4888. |
||
|
|
||
|
healthexecwire |