

Click here
to view this message in a web browser
 |
||
| Understanding Medicare’s Use of Episode-Based Alternative Payment Models | ||
|
There has been a great deal of uncertainty
in recent months surrounding the use of episode-based payment models at
CMS. The voluntary Bundled Payments for Care Improvement (BPCI) models
have been operational since 2012, and the mandatory Comprehensive Care
for Joint Replacement (CJR) program was implemented in April of 2016 and
has hundreds of participants nationally. However, since the beginning of
2017 CMS has issued proposed and final rules that created and
subsequently cancelled three new Medicare Parts A and B episode payment
models. Milliman has analyzed the major provisions of these final rules
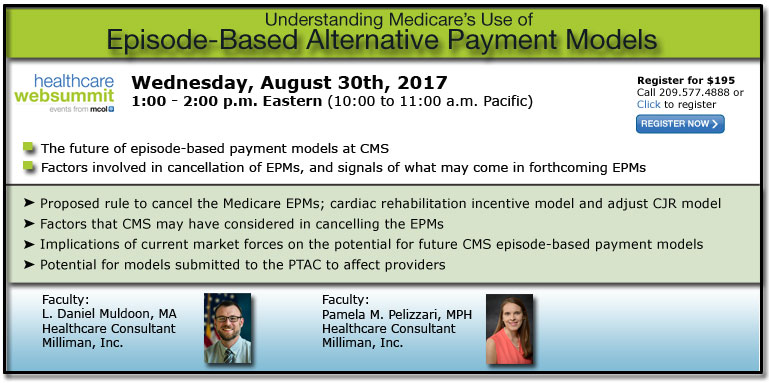
and considered the potential implications for affected providers. Despite the recent cancellation of the three EPMs, CMS has still signaled strong support for episode-based payment models. There continues to be a large number of participants in the voluntary BPCI models, and CMS has signalled that they intend to introduce a new version of that model by the time it expires in October 2018. Furthermore, a large number of episode-based payment models are being submitted to the Physician-Focused Payment Model Technical Advisory Committee (PTAC), which has been tasked with considering models submitted by stakeholders for possible implementation by CMS. In this session, we will consider the future of episode-based payment models at CMS. We will discuss the factors that may have led to the cancellation of the EPMs, as well as signals of what may be to come in forthcoming episode-based payment models. Please join us Wednesday, August 30th, 2017 at 1 PM Eastern as Milliman's Daniel Muldoon and Pamela Pelizzari discuss this topic. Click here for detailed information and to register or call 209.577.4888. |
||
|
|
||
|
healthexecwire |